As healthcare in the United States changes, health insurers must change with it. Many realize this and have begun implementing new initiatives, both on their own and per regulatory mandates. One critical item insurers must address is their relationship with consumers in the near future.
Currently, many consumers are wary of their health insurance companies. The employer-based model means that most end user consumers have little to no say in how their insurance plan is chosen, and therefore sometimes feel that their own healthcare may be out of their control. Actions by health insurance companies certainly add to this unease. Consumers in general are frustrated by their overall experience with their health insurer.
Additionally, forces affecting the healthcare ecosystem are driving several key consumer trends. Reform and regulations, as well as new pricing and plan options, mean that more consumers are entering the system. At the same time, the overall healthcare system is growing in complexity, also due to reform and regulations. In addition, consumers are starting to acquire a larger role in decision-making about their insurers, plans, providers, and treatments, with increasing influence over aspects of their health, such as prescriptions, healthcare delivery, and payments. And more of the financial burden of healthcare is put on consumers' shoulders, either directly or indirectly.
As a result, consumers' needs are changing and health plans must adapt. Consumers want more information, including new types of information and greater levels of detail. They also demand more in-depth interactions and more immediate access to providers, insurers, and data. They expect healthcare providers and insurers to provide better tools to use in managing decisions about their health, as they define it, and they value products and services that support their "world view" of health and of their healthcare.
Peppers & Rogers Group has outlined five key challenges facing health insurers today brought about by these changes, as well as by customers' evolving expectations. Companies that work to overcome these challenges will not only have a competitive advantage, but also will be in a position to provide better customer experiences and operate more efficiently than in the past.
1. Develop actionable consumer insight
Consumers want to be treated like people, not policy numbers. They want their health insurer to connect with them on a personal level. Many want their insurers to be a trusted advisor that can educate, but not overwhelm them with information and choices. Where appropriate, health insurers should work with individuals to find the right coverage and help them save money, while also guiding them to improve their health and reward their behavior. Patient trust is critical, and the way to earn that trust is to understand individual consumers.
Therefore, we recommend that companies invest in understanding the needs, behavior, and value of groups within a company's consumer base. Needs analysis will uncover common consumer attitudes, beliefs, and motivations, while behavioral analysis using transaction (claims) and interaction (channel) data will show how consumers generate value. Additionally, predictive customer lifetime value models can help a firm understand the current and future value of individual consumers. This internal customer insight forms the basis for a relationship strategy and interaction plan that can't be matched by competitors because they don't have the insight used to create it. The plan should include prioritizing and customizing sales, marketing, and service interactions with different customer groups in a way that benefits both the consumer and the company.
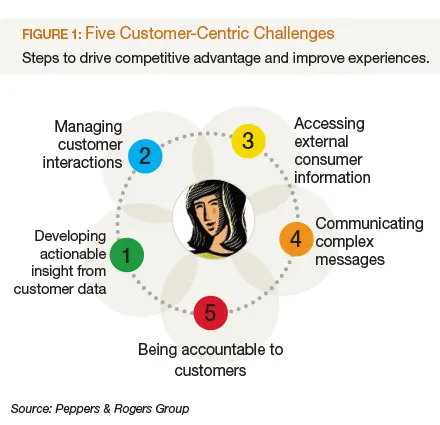
2. Manage interactions with customers to deliver a satisfying customer experience
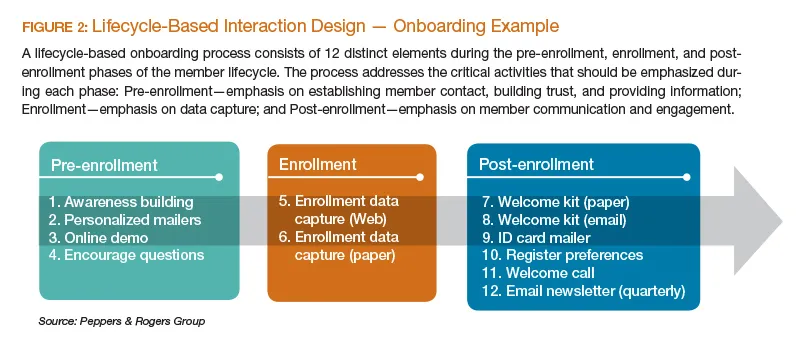
Consumers are offered myriad interaction choices. The experience within and across those channels goes a long way to influencing customer satisfaction and loyalty, as well as improving efficiency and effectiveness on the part of the organization. To further enhance their interaction plan, insurers need to understand all the touchpoints and interactions consumers have with the company, and then establish lifecycle-based interaction plans to optimize those interactions.
Once again this is where the importance of customer insight cannot be understated. We suggest that companies map out every possible customer interaction point visually via a customer touchmap, then develop a customer experience design program that includes lifecyclebased interaction plans derived from needs, value, and behavior data. The program should include value propositions, treatment strategies, and optimal customer experiences at every possible interaction point.
3. Access consumer information and use external data to make decisions and recommendations
The healthcare space is one driven by data. Whether it is electronic health records, drug information, treatment histories, or other data, health insurers collect reams of potentially useful information. Reconciliation and analytics are necessary to make sense of what could be an overwhelming amount of data.
We recommend matching customer information, observed and acquired, with data from transactional systems and outside industry data. Through data mining, modeling, and other analysis, companies can gain additional insight and take action on the basis of in-depth knowledge acquired through that mix of internal and external information.
Adding processes and systems like a centralized data warehouse and CRM program will allow stakeholders to access customer data seamlessly across touchpoints and over time. For example, an insurer may combine current data with predictive analytics and decision management tools to build new campaigns and processes that enables the firm to make individual recommendations based on facts, not hunches.
4. Communicate complex messages to create a clear and productive dialogue
Much of the language used between health insurers and consumers is confusing, adding complexity to an already complex relationship. As the adage goes, it's not what you say, but how you say it that counts.
We suggest that, in addition to more traditional modes of communication, companies use social media and mobile communications to clearly communicate complex messages. For example, businesses can use community forums, social networks, videos, FAQs, searchable knowledgebases, co-branding, partner links, and the like to disseminate information to consumers. Simplifying the message is also often an overlooked option.
A thorough communication audit and language alignment may be in order, to ensure consistent and clear messaging between the insurer and consumers. We also recommend using all the customer insight gathered to create relevant, targeted messaging, which is much more likely to resonate with consumers and drive action than generic messaging.
5. Be accountable
The world is becoming increasingly transparent as information is more widely available to more people. This is true in the healthcare industry, as well. Consumers look for accountability and will be vocal when they do not find it. Proactive companies embrace this new reality. Accountability requires more than a mind-set shift. It requires internal change management and investment in resources to enable accountability. Consequently, we recommend that companies provide employee training and education on products and services, empower all employees to resolve issues, and use incentives and measurements such as Net Promoter Score, customer satisfaction, and Return on Customer to track success.
Customer centricity is an industry-wide imperative, but is not a sure source of competitive advantage for everyone. A clear understanding of an organization's business model, along with detailed short- and long-term goals, will help clarify whether this approach will benefit a firm's specific circumstance. Competition among insurers will drive some of them to invest in different business models. And other healthcare players, along with some currently from outside healthcare like technology companies, will present new competitive challenges. The more business leaders understand the needs of their organization and the individual consumer, the better prepared they will be to face those challenges and succeed in the new healthcare landscape.

















